This post is a tad off-topic but one that I think is too important not to share – perimenopause. It directly affects half the population and arguably indirectly affects the other half. Men and younger women, if you’re anything like me, I previously ignored anything to do with menopause as I thought – I’m too young for that/doesn’t concern me, I’ll worry about that when I get there. Wrong. Men, there are things to be aware of to support the women in your life and younger women, there are things you can be doing in your early 30s to reduce effects, live longer and increase vitality. Symptoms can also start occurring much earlier than you’d think.
In my usual hyperfocus mode – I’ve devoured a decent amount of content that I’d like to summarise including what perimenopause is, its symptoms and things you can do in your 30s to reduce effects, live longer and increase vitality. I am obviously not a doctor and am just compiling a summary of what I’ve read (sources below) – please consult a relevant professional before implementing anything. This 20-minute read consolidates the key take-aways from a number of hours of content so hopefully it’s of use.
To put a financial independence spin on it, studies show that 1 in 5 women will quit their jobs because of menopause symptoms. That’s a staggering number with a huge economic impact on the women themselves, their families and the companies they work for. I also think that striving for financial independence at a younger age will allow for the time needed to implement the various strategies to reduce the symptoms of menopause before they occur.
Table of Contents
Definitions:
Menopause:
Menopause is currently defined as one day, exactly one year after your last period. It represents the end of ovarian function. Women are born with all their eggs (1-2 million at birth), by 30 we are down to 10%, by 40, 3% and the quality is declining. Menopause is when no eggs are left. No or very little sex hormone production will come from the ovaries, and estradiol levels decline to about 50% or less of your healthiest years.
Perimenopause:
The time leading up to menopause. Hormones wildly fluctuate causing psychological and physical changes to occur, including the length of time between periods.
Postmenopause:
This starts the same day as reaching menopause. Despite no longer having periods, varying degrees of symptoms still occur. Hormonal swings settle down and some symptoms may improve. However, with the absence of estrogen, women face increased risks for heart disease, osteoporosis (bone loss) and dementia. Because of increased life expectancy, women can expect to spend 40% of their lives post-menopause. Keep reading to see what you can do to reduce these risks.
When can it start:
The average age of menopause is 51-52 but can range from 45-55.
Perimenopause starts 7-10 years before the last period – or 8-11 years before you reach menopause since menopause is 1 year after your last period.
So you could well be 34 when you start to experience perimenopause symptoms.
What’s really going on:
Before getting into the symptoms, this is the science bit about what is actually happening in endocrinology in the body.
A normal healthy menstrual cycle before menopause has a reproducible monthly rise and fall of estrogen, progesterone and brain hormones LH (a chemical in your body that triggers important processes in your reproductive system), FSH (a hormone your pituitary gland makes and releases that plays a role in sexual development and reproduction) and GnRH (the key regulator of the reproductive axis).
The hypothalamus in the brain has a sensor looking for estradiol levels and when they get low it sends GnRH down to the pituitary which sends out pulses of LH and FSH which tells the ovaries to ovulate. The process of ovulation drives estrogen levels back up.
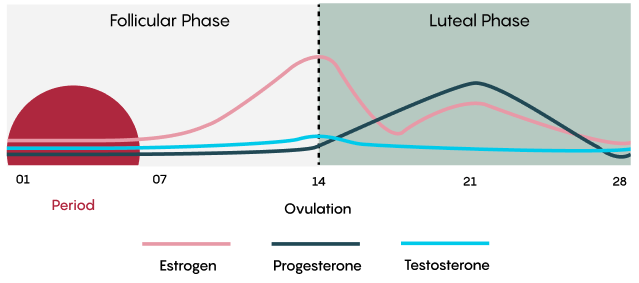
When we reach perimenopause, the egg supply is low and the signals don’t work as well. We start becoming resistant to the LH and FSH surges so the brain sends more FSH and the ovary eventually gets the egg out but sometimes it’s delayed so the timing of the previously predictable cycle gets out of whack. Sometimes they are closer together, sometimes further apart.
Estrogen and progesterone levels start changing dramatically. Estrogen surges are much higher than before and lows are lower than before.
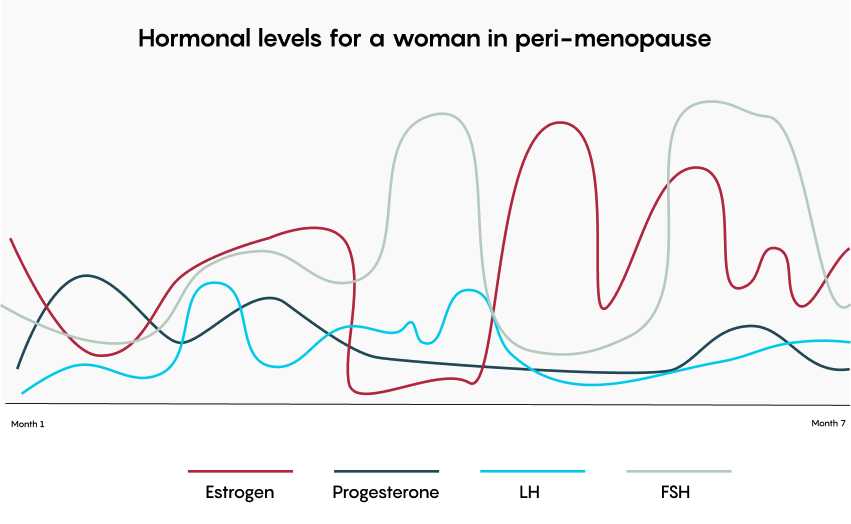
Hormonal chaos.
This is why there is no reliable blood test to diagnose menopause. Most are diagnosed through symptoms.
In regards to hot flashes (vaso motor symptom), these are caused by a dysregulation of the thermoregulatory centre in the hypothalamus, the thermostat gets reset and causes vassal dilation. It starts in the core somewhere in the chest/neck area and goes up into the neck and out into the extremities, then you start sweating profusely from all the blood vessels dilating which can last minutes. For some women, it’s preceded by palpitations or intense feelings of dysphoria/ sadness.
Symptoms:
Symptoms vary from person to person both in the symptom itself, the duration and the severity of it.
Approximately 85% of women experience menopausal symptoms. 25% of women experience severe symptoms, 25% find symptoms to be mild and the remainder are somewhere in between.
That said, before you get too discouraged, there are actions you can take both before you get there and when you’ve reached perimenopause to better manage and even reduce these symptoms. An ounce of prevention is worth a pound of cure.
As you will see by the list below, menopause can mimic other ailments/diseases so it’s important to rule those out first so you’re addressing the correct root cause. To help your doctor, it’s important to track symptoms over a period of time to see trends and cyclical activities.
The biggest early indicator is mental health changes. The brain does not like the chaos of the hormonal swings. Neurotransmitters are very sensitive to estrogen, progesterone and testosterone. These swings can result in deviations from normal levels of serotonin (influences learning, memory, and happiness as well as regulating body temperature, sleep, sexual behaviour and hunger), norepinephrine (mobilizes the brain and body for action) and dopamine (motivation, feel-good hormone). As the hormone swings become chaotic there is an increase of at least 40% of mental health disorders.
Changes can look like: suddenly feeling less optimistic, increased anxiety/panic attacks, loss of executive functioning/ADHD-like symptoms (brain fog, loss of words, difficulty concentrating, not being able to do calculations) which result in a lack of confidence at work (see stat about women leaving the workforce above).
Other symptoms can include:
- Acid reflux/GERD worsening
- Acne
- Allergies (new, different)
- Atrophic vaginitis/genitourinary syndrome of menopause GSM (or vaginal atrophy, drying and thinning of the vaginal walls)
- Balance issues
- Bloating
- Body odour (changes)
- Body aches (random come/go)
- Breast soreness
- Brittle hair and nails
- Burning mouth (decreased saliva)
- Cold flashes (more common at night)
- Depression
- Digestive problems (IBS, bloat, gas)
- Dizziness (vertigo)
- Dryness (skin, mouth and eyes)
- Exaggerated PMS symptoms (bloating, breast pain, cramps)
- Fatigue
- Gum/dental problems
- Hairloss
- Headaches
- Heart racing/palpitations (irregular heartbeat)
- Hot flashes
- Increased cortisol levels (slows digestion/contributes to constipation)
- Increased hair growth on other areas of the body (face, neck, chest)
- Increased tendon and ligament injury
- Intolerance to some foods (changing tastes)
- Irregular periods (missed periods, longer/shorter, heavier/lighter, flooding, spotting, clotting, dark/different coloured blood)
- Itchiness (overall skin, also links to paresthesia)
- Low/decreased libido
- Memory lapses (brain fog, forgetfulness)
- Migraines
- Mood swings (crying jags/sadness, anger/rage)
- Muscular skeletal issues: hip pain, joint pain (stiffness, frozen shoulder, increased inflammation), back pain with no related injury
- Muscle tension
- Muscle mass loss (sarcopenia)
- Nausea
- Night sweats
- Osteoporosis (reduced bone density)
- Reduced ability to process alcohol, drastically impacts sleep
- Restless Leg Syndrome
- Sense of smell changes
- Skin crawling (feeling something crawling on your skin)
- Sleep disruption (lack of sleep)
- Spatial awareness changes (proprioception, more clumsy)
- Stress incontinence
- Swelling of hands/feet
- Thyroid changes
- Tingling extremities
- Tinnitus
- Unexplained irritability
- Urinary Tract Infections (UTIs)
- Weight gain (low estrogen levels promote fat storage in the belly area as visceral fat)
In addition, if you have any existing conditions like IBS/GERD, arthritis, inflammatory diseases, ADHD, autism or bipolar, the symptoms of those conditions can also be further aggravated/worsened.
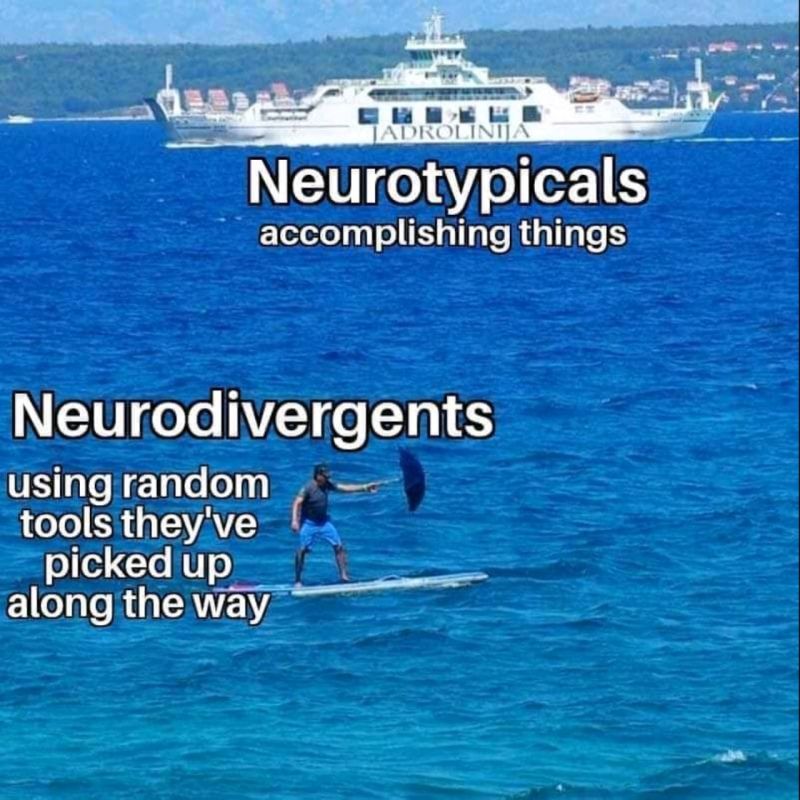
A lot of neurodivergent women are getting diagnosed for the first time in perimenopause as symptoms are so exaggerated and the coping mechanisms they’ve cobbled together over the years are no longer effective.
Other Important Notes:
Estrogen is protective.
Loss of estrogen accelerates the path to cardiometabolic diseases. Risk of heart disease, osteoporosis and stroke increase post menopause due to loss of estrogen.
Estrogen is neuroprotective
The longer your body is exposed to estrogen (natural or otherwise), the higher your cognition scores and the healthier the brain. The decline in estrogen is correlated with neurodegeneration.
The older you are when you go through menopause, the healthier you are for cardiometabolic disease.
Certain factors can cause you to go through menopause sooner including:
- If you smoke
- If you don’t have children (more ovulation runs through supply faster)
- If you have a hysterectomy without removing ovaries, you lose 4 years off the life of your ovaries
- If you have tubal ligation, you lose a year and a half
- If you’re African-American, you can go through a year and a half sooner
- If you have chemotherapy
- If you have surgery
- If you have any inflammatory process in the abdomen (irritable bowel or endometriosis) you will lose some of the life of the ovary
On the flip side, you may go through menopause later if you:
- Are Asian (1-2 years later)
- Have taken birth control that stops ovulation for 5 years or more (can push out by about 9 months) – that said there are many other considerations around the pill that should be considered.
Body composition changes in perimenopause without changes in diet or exercise.
Pre-menopause, about 8% of your fat is visceral (fat around your internal organs), after the transition it shifts to 23% without changes in diet or exercise. Visceral fat is a harbinger of chronic disease. We also lose muscle. The muscular-skeletal system (bone and muscle) works together, muscle controls our basal metabolic rate which determines resistance to insulin so muscle loss causes all kinds of issues.
Visceral fat is hard to lose.
It’s possible to lose but it’s hard work. The more you can reduce this BEFORE you go into perimenopause, the better your outcomes will be.
There are scanners that can identify how much visceral fat you have but a rudimentary method is to measure your waist-to-hip ratio. Take the measurement of your waist and divide it by the measurement of your hips. If it’s less than 0.7 then your chance of having clinically significant deviations in visceral fat are low. If greater than 1, you likely have higher levels of visceral fat.
Hormone replacement is better than anti-depressants to treat menopause-related depression.
Currently, SSRI use doubles across the menopause transition, however, data is now showing that hormone replacement therapy lowers the onset of depression and is a better treatment than SSRIs if depression has occurred as it treats the root cause which is a drop in estrogen.
Research into perimenopause is lacking.
If you go to PubMed – a source of 37 million citations for biomedical literature from MEDLINE, life science journals, and online books – and type in pregnancy, 1.1 million articles come up, menopause brings up 97,000 and perimenopause brings up 6,400.
Women are living longer than men but 20-25% of that is in poor health.
The higher your protein intake, the less likely you will be frail in old age.
When your mother or aunts went through menopause and any medical conditions they experienced are a big indicator of when and how you will experience menopause.
Loss of sex hormones in menopause changes the gut biome from a typical female microbiome to that of a male.
Changes in the gut microbiome can result in result in all kinds of changes. You could be eating the same foods as before but your gut is not handling them as it used to. More bloating, insensitivities etc.
Intermittent fasting can make it hard to intake the volume of protein we need to maintain muscle mass.
Metabolizing protein is its own work so it’s best to spread it out throughout the day. It’s best to break protein intake into nuggets throughout the day. Don’t just have a big protein portion at dinner. Have bits at breakfast and lunch too. Fasting can make it hard to do that.
50% of women will have an osteoporotic fracture before they die
Men are about half that.
If you break a hip over the age of 65 you have a 30% chance of death in 1 year with surgical repair, and a 79% chance without surgery.
Reduce this risk by strengthening muscles and bones. Do resistance training 3 times a week. Eat more protein. Take collagen and creatine supplements.
Any women at any point in the menopause journey has a 50% sexual dysfunction rate.
Meaning she is not happy with whatever is going on. This can be delayed orgasms, lower orgasm peaks, loss of elasticity in the skin resulting in painful sex, lack of arousal symptoms, relationship disorder (don’t love your partner or don’t feel supported), low libido etc. See solutions below.
Solutions:
In general, the healthier you are going into perimenopause, the better the course is going to be for you.
Here are some of the things you can do, both before and during perimenopause to reduce symptoms.
- Nutrition
- in particular a Mediterranean, anti-inflammatory diet, estrogen is an anti-inflammatory hormone, so in perimenopause, that declines and we lose that protection, diet is one of the most important things that determines your level of inflammation
- most of your food should be unprocessed/minimally processed which allows you to get plenty of vitamins, minerals, probiotics and micronutrients that we all need for physical and mental health
- more fibre (fruits, veggies, whole grains, beans and legumes): most women are getting 10-12 grams a day, we need at least 25. Fibre feeds the gut microbiome slowing down glucose absorption, pulls more water into the gut and all kinds of other health benefits. A good guide is to eat as many different plants in as many colours as you can as often as you can. Here are some tips on how to get 25g of fibre a day
- more probiotics: prebiotics (fibre) + probiotics (fermented foods/yogurt) = postbiotics (health-inducing compounds produced by gut microbes). The probiotics introduce healthy bacteria for our gut microbiome, the fibre acts as a fuel to feed those healthy gut bugs and together they create a healthy gut microbiome which has all kinds of health benefits including reduction in menopausal symptoms. Although you can take probiotic supplements, the best and most effective will be what you eat. Probiotics can be found in things like sauerkraut, kimchi, miso, yogurt, unpasteurised fermented pickles etc.
- more protein: as above, we need to maintain our muscle mass. Protein helps build muscle. Women are generally getting 50-60 grams a day. We likely need 80-120 depending on body composition or 1g per pound of body weight. Here are some tips on how to get there
- Sleep (good sleep hygiene/routine)
- If you have a good sleep hygiene and routine already established going into perimenopause it can help reduce symptoms
- If you’re having hot flashes or other sleep disturbances, things like hormone therapy can help to get the thermal regulatory centre and serotonin levels back to normal
- If you’re on HRT and still having middle-of-the-night awakenings, racing thoughts or get up to pee and can’t get back to sleep, something like progestin might help to settle down the brain
- For better sleep, cut out alcohol or at least know that if you are choosing to drink, you are choosing alcohol over quality sleep
- Regular exercise (in particular resistance/strength training)
- Diet and exercise with the goal of being thin can actually chip away at bone and muscle strength needed to stay fit into old age. Research is now showing that everyone, male, female, young, old, should resistance train at least three times a week
- Use of a weighted vest may be an easy way to start building this in while walking
- Stress reduction: Keeping cortisol levels down will make you healthier in every other way
- Supplements: Vitamin D, Creatine for muscle (5g/day), Bioactive collagen for bone density
- Acupuncture: This can help reduce symptoms but is expensive and not addressing the root cause which is a decline in estrogen
For sexual dysfunction:
- Vaginal estrogen therapy can help where sex hurts
- Viagra can help where you want to do it but the blood’s not getting to where it needs to go
- If your relationship is struggling, therapy can help
- If you previously had a good libido, you have a good relationship with your partner and it doesn’t hurt, then testosterone can help
Mental health:
This last one is a hunch of mine based on what I’ve read in books like The Myth of Normal and accounts of women who have gone through menopause, so take of it what you will, but I do believe that any unresolved mental health issues, be it trauma or unprocessed emotions or grief to name a few, will come to the surface in menopause. So any work you can do before you reach perimenopause in respect to counselling or other therapies to process and release those emotions will only help to reduce symptoms and make you more resilient.
Some studies show that neurodivergent women will experience menopause symptoms more severely. My gut tells me that part of this is because neurodivergent women typically experience more trauma and have a very low window of tolerance in their nervous systems. As a lot of women are late diagnosed, it is also unlikely we will have done the relevant therapy to process and release that trauma or built up resilience in our nervous systems, hence the experience of increased symptoms in menopause. Again, just a theory but I’m hoping that the work I’ve done in this space will pay off.
Hormone Replacement Therapy
That WHI study:
Hormone replacement therapy got a bad reputation resulting from the misrepresentation and misinterpretation of a medical study that was completed by the WHI (Women’s Health Initiative) in 2002.
The data that caught the headlines was misinterpreted and stated that HRT causes a 25% increased chance of breast cancer but in actuality, the absolute risk was an increase of 0.8%. In addition, the study was done on women who were already 10-13 years post-menopausal which can be argued were already past the point of the preventative benefits that estrogen can provide.
Unfortunately, many doctors and even specialists are now refusing to prescribe HRT because of this study. You may be able to find supportive physicians in your area here.
In contrast, in 2020, a different study found that women who started HRT between 50 and 59 had a 50% decreased risk of cardiovascular disease and death from cardiovascular disease and all-cause mortality. Estrogen is better at prevention than cure. It’s protective of the coronary arteries so taking estrogen away, we lose that protection and disease and plaque can start to build up so there is a worry that adding estrogen once you’ve developed sclerosis or plaque might loosen the plaque which can lead to slightly increased risk of stroke so it’s important to get the right tests and scans before starting.
HRT or not?
Not every woman will choose HRT but every woman deserves an informed conversation about it and let her make her choice.
It’s a bit like when I took Little MH for his vaccines – there is a booklet that says getting this vaccine has these risks but not getting the vaccine and actually catching the disease has these much greater risks up to and including death.
So HRT has a small risk of breast cancer but lack of estrogen increases cardiovascular disease, diabetes and insulin resistance and increased cholesterol. Statistics show that the most common cause of death of women is cardiovascular disease, heart attack or stroke. So framing it this way can help to shift the perspective.
On cholesterol: 80% of women will have abnormal cholesterol levels through menopause. Elevated LDL and lowering HDL means greater risk of cardiovascular disease. Statin is typically prescribed. In 2020, it was found that Statin does not decrease risk of primary heart attack in women (though it does for secondary) and does not decrease risk of death from cardiovascular disease but as above, if given in the right window of opportunity, HRT does.
Side note:
The difference between low-dose birth control pill and high-dose hormone replacement are not that far apart.
Heart Attack Signs in Women
On the topic of heart attacks, did you know women are much more likely to die in a hospital setting from a heart attack than a man because we don’t present the same symptoms as men do?
Women experience more psychological symptoms rather than the biological symptoms that men do. As a result we are more likely to brush them off and delay going to the hospital.
Symptoms can include:
- Neck, jaw, shoulder, upper back or upper belly (abdomen) discomfort.
- Shortness of breath.
- Pain in one or both arms.
- Nausea or vomiting.
- Sweating.
- Lightheadedness or dizziness.
- Unusual fatigue.
- Heartburn (indigestion)
Sources:
- Andrew Huberman Podcast with Dr. Marie Claire Haver
- The menopause wiki
- Fibre Fuelled by Dr. Will Bulsiwicz
- The Myth of Normal by Dr. Gabor Mate and Daniel Mate